Link Between NAFLD and Heart Failure – A Cardiology Perspective
INTRODUCTION ABOUT DR. Marat Fudim
In this insightful webinar on Non-Alcoholic Fatty Liver Disease (NAFLD), we are joined by Dr. Marat Fudim, a distinguished cardiologist and heart failure specialist based at Duke University, United States. He will shed light on the increasingly evident link between NAFLD and heart failure, a relationship of great significance to the global healthcare community.
OVERVIEW OF THE Link Between NAFLD and Heart Failure
Table of Contents
- The Emerging Epidemic: Non-Alcoholic Fatty Liver Disease (NAFLD)
- NAFLD: A Multisystem Disease
- Association of NAFLD with Cardiac Structural/Functional Changes
- Meta-Analysis of Incident Risk of HR after NAFLD
- The Emerging Epidemic: HFpEF
- Association of NAFLD and HFpEF: Phenotypes
- Obesity HFpEF – Also known as Metabolic HFpEF Phenotypes
- Screening for NAFLD
- Why do we care about fibrosis?
- Components of a Lifestyle Approach to NAFLD
- Pharmacotherapy for NAFLD: Current Scenario and Approaches
- Future Directions in NAFLD Pharmacotherapy: Mechanism of Action
- Key Insights to Remember from Dr Marat Fudim
The Emerging Epidemic: Non-Alcoholic Fatty Liver Disease (NAFLD)
Dr Marat Fudim initiates the conversation by spotlighting the burgeoning non-alcoholic fatty liver disease epidemic. NAFLD is a pervasive health issue with staggering prevalence rates. Depending on the region, between 25 to 50% of a given continent’s population has been associated with prevalent NAFLD. This prevalence is not uniform globally and varies from region to region, but these figures are undeniably high, largely driven by the concurrent obesity and diabetes epidemics.
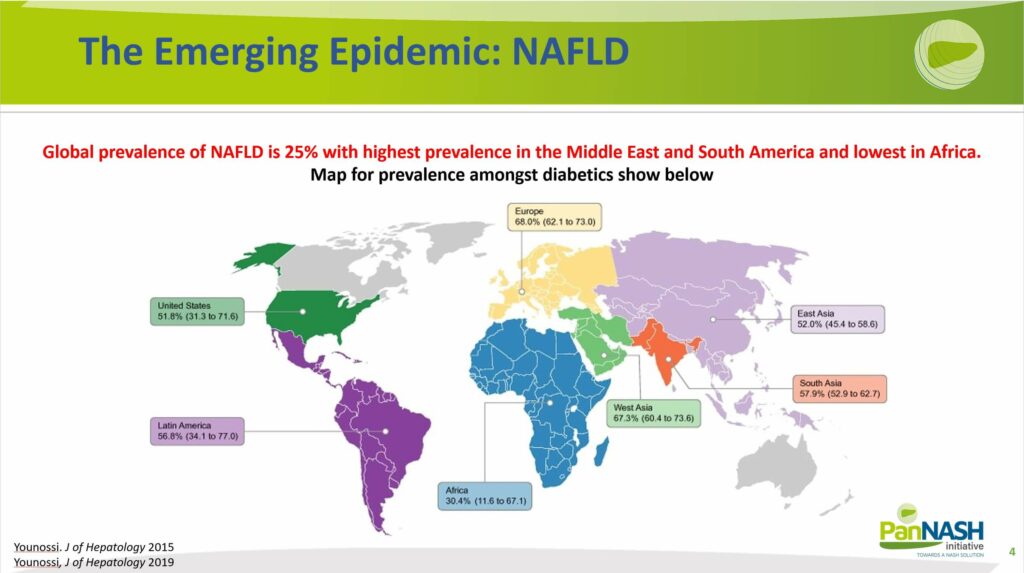
Dr Fudim highlights the significance of the increasing incidence (A) and the widespread prevalence (B) of NAFLD. As illustrated, NAFLD is a broad term encompassing various degrees of liver disease, making its prevalence a critical public health concern.
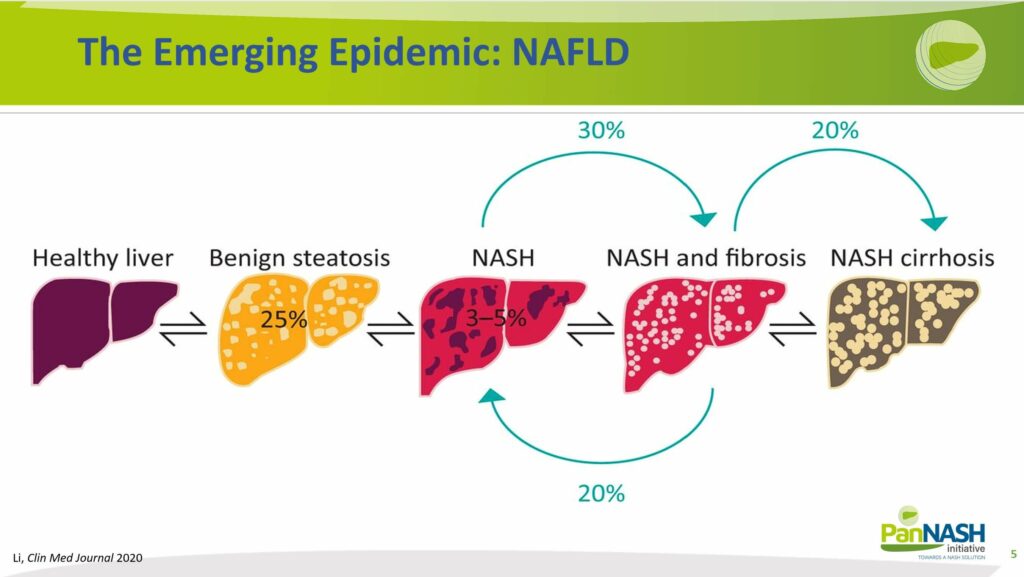
If benign steatosis, or the harmless accumulation of fat in the liver, occurs in approximately 25% of the population, there is a substantial risk that a significant portion of these patients will progress to non-alcoholic steatohepatitis.
NASH can subsequently lead to varying degrees of fibrosis, potentially progressing to cirrhosis. At this stage, the disease might or might not be reversible and could require a liver transplant. As depicted in the graphics, this is a situation we would ideally want to avoid, underscoring the need for early detection and management.
NAFLD: A Multisystem Disease
Switching gears, Dr. Fudim offers a cardiologist’s perspective on the interlink between non-alcoholic fatty liver disease (NAFLD) and heart failure.
The concern arises from the fact that many risk factors leading to NAFLD, such as metabolic syndrome and hyperlipidemia, also contribute to cardiovascular issues.
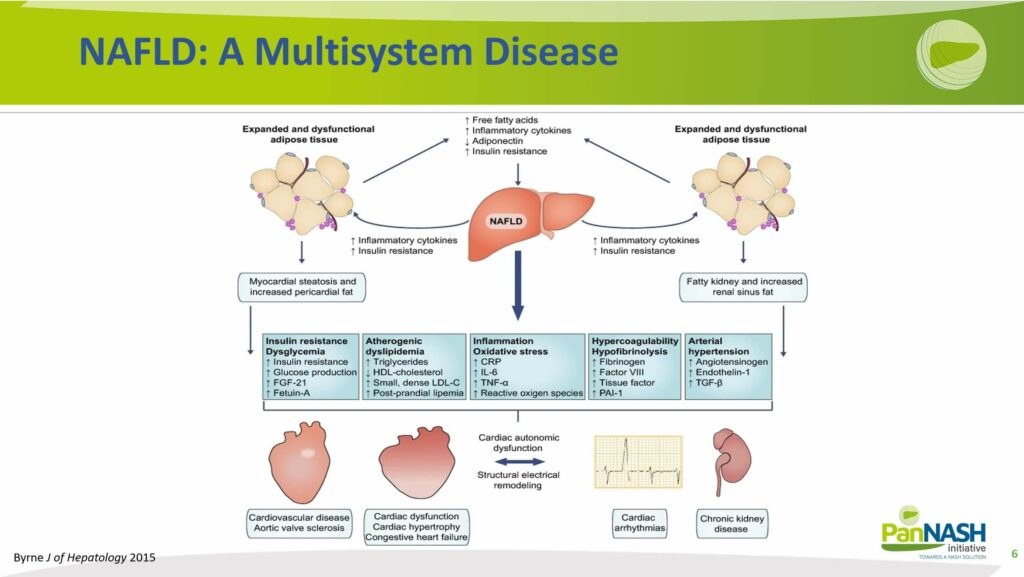
Moreover, the consequence of an affected liver might infect the global systemic activation of the inflammation system. It might also change the factors produced by the liver adversely, in most cases to the detriment of the individual’s health. These changes lead to the key components that affect the cardiovascular system.
Firstly, insulin resistance tends to increase, enhancing the propensity for metabolic syndrome and diabetes.
Secondly, the condition can make a person more pro-atherogenic, increasing the likelihood of developing coronary or peripheral vascular disease. The systemic inflammation associated with NAFLD can also make the individual more prone to hypercoagulability.
Furthermore, NAFLD can lead to greater systemic hyperactivation of the vascular system, resulting in higher instances of arterial hypertension.
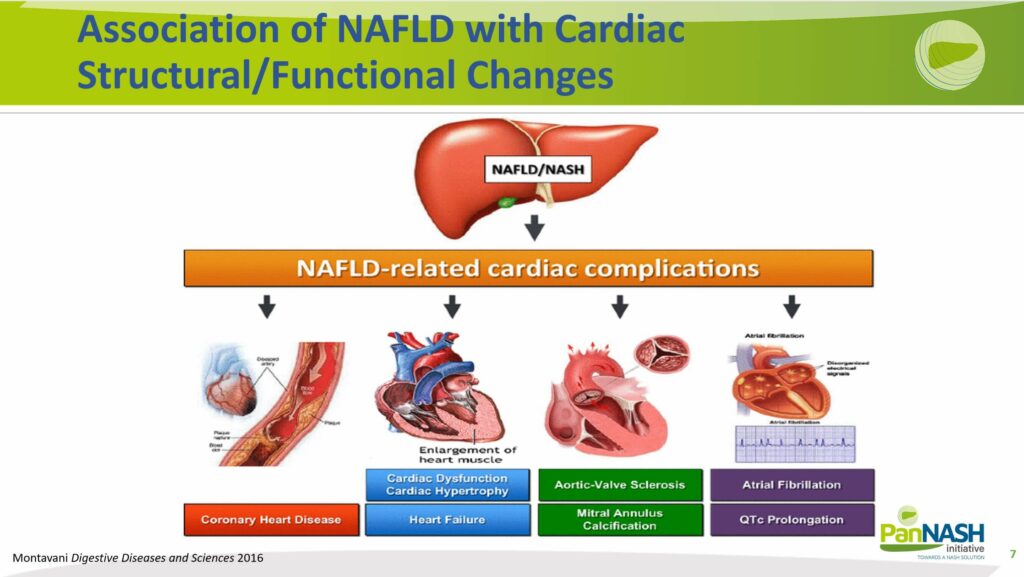
Association of NAFLD with Cardiac Structural/Functional Changes
The cumulative effect of these factors significantly heightens the risk for downstream cardiovascular complications. Each component individually contributes to this heightened risk – for instance, there’s a notable increase in the likelihood of developing coronary artery disease (CAC).
There is a well-documented association between NAFLD and various cardiovascular conditions, including left ventricular hypertrophy, valvular disease, increased incidence of arrhythmias, and heart failure.
Meta-Analysis of Incident Risk of Heart Failure after NAFLD
Upon examining the incidence of heart failure, as highlighted in a recent publication, we discovered a noteworthy rise in new cases of heart failure. This trend was evident regardless of whether the heart failure was characterized by reduced or preserved ejection fraction, a distinction we did not focus on in this particular study.
Our focus was on individuals without NAFLD in the registry, encompassing global records from Asia, Europe, and the US. We observed that the incidence, or the new onset of heart failure, was around 60% within the subsequent five to ten years.
This represents a significant number of new-onset heart failure cases, considering the substantial prevalence of NAFLD, estimated to be around 25%. By simple calculation, one can comprehend the magnitude of the issue, which translates to millions of patients developing heart failure as a result of NAFLD.
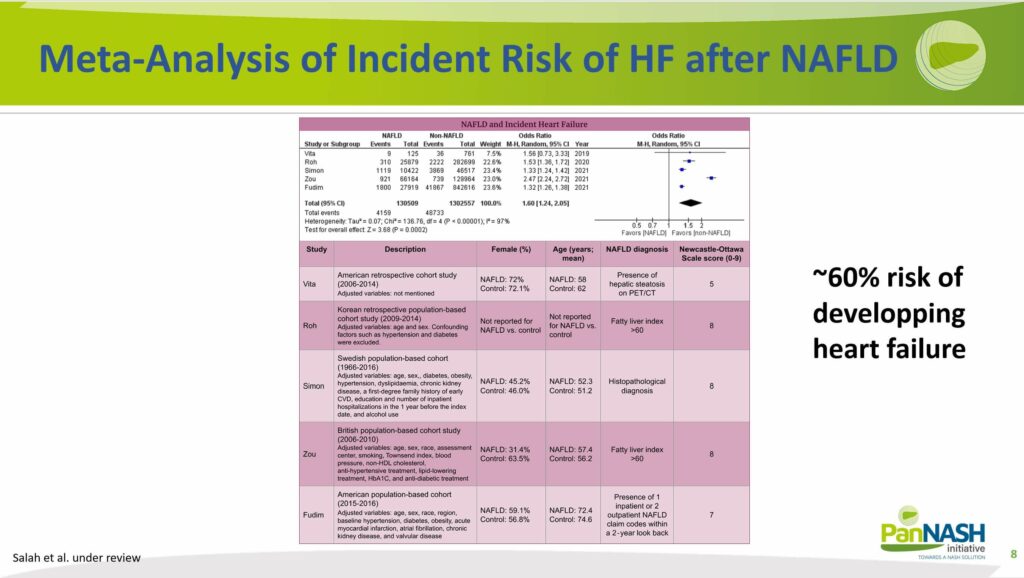
An intriguing discovery from a subsequent analysis revealed that, in most instances, these patients suffered from heart failure with preserved ejection fraction (HFpEF). This was elaborated in a separate presentation Dr Fudim conducted, wherein he emphasized the connection between NAFLD and HFpEF. Notably, HFpEF is primarily the disease within heart failure that is driven by NAFLD.
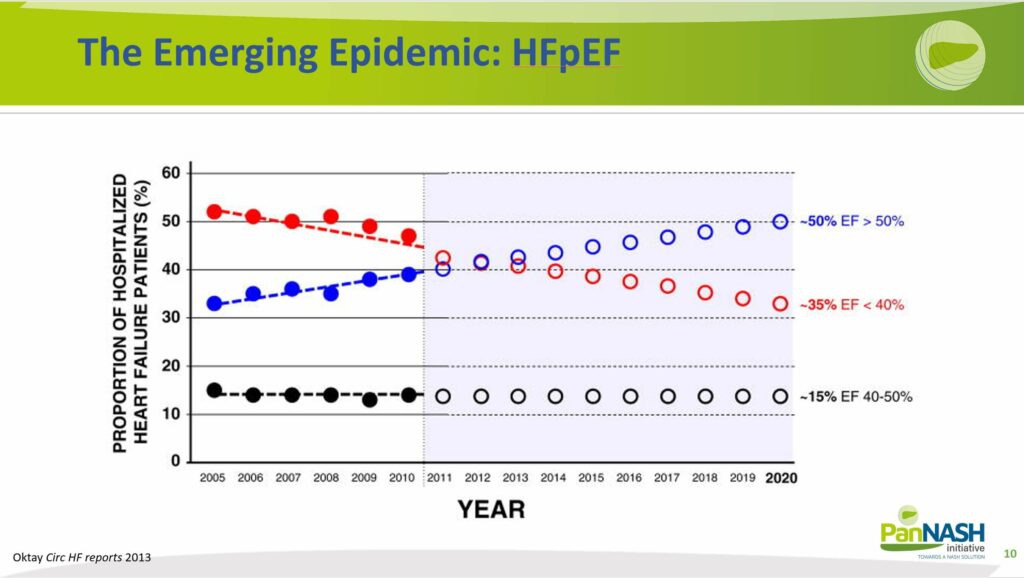
The Emerging Epidemic: HFpEF
It is well-established now that heart failure with preserved ejection fraction (HFpEF) and heart failure with reduced ejection fraction (HFrEF) each comprise about half of the heart failure population in the US, a trend likely mirrored globally as well.
However, a paradigm shift is anticipated, with HFpEF predicted to represent 70% of heart failure cases and HFrEF the remaining 30%. This shift is predominantly fueled by the escalating prevalence of NAFLD and the concurrent obesity epidemic. The evidence strongly suggests that the majority of HFpEF cases are driven by these two interlinked public health crises.
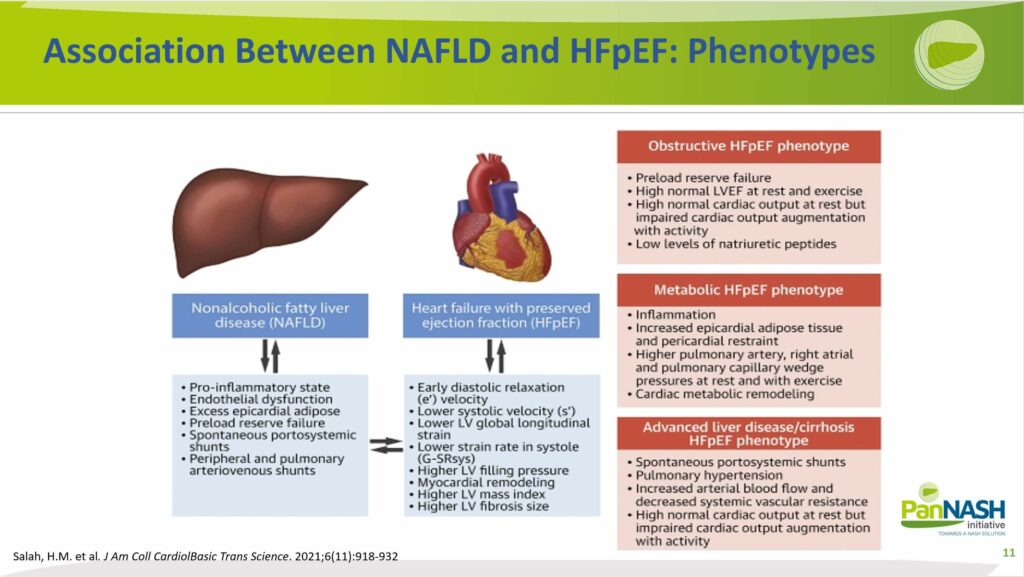
Association of NAFLD and HFpEF: Phenotypes
Recognizing that the presentation of NAFLD-induced heart failure isn’t uniform is essential. Heart failure is an extremely heterogeneous disease, and the identification of a co-existing liver disease or potential liver disease driving heart failure could be crucial.
Based on the recent publication of Dr Marat, there might be several different phenotypes of heart failure, specifically heart failure with preserved ejection fraction (HFpEF). They are the obstructive, metabolical or advanced liver disease phenotypes. At the same time, it’s crucial to target and treat liver disease concurrently, and it’s important to acknowledge that the degree of liver and heart contributions at that time point varies dramatically.
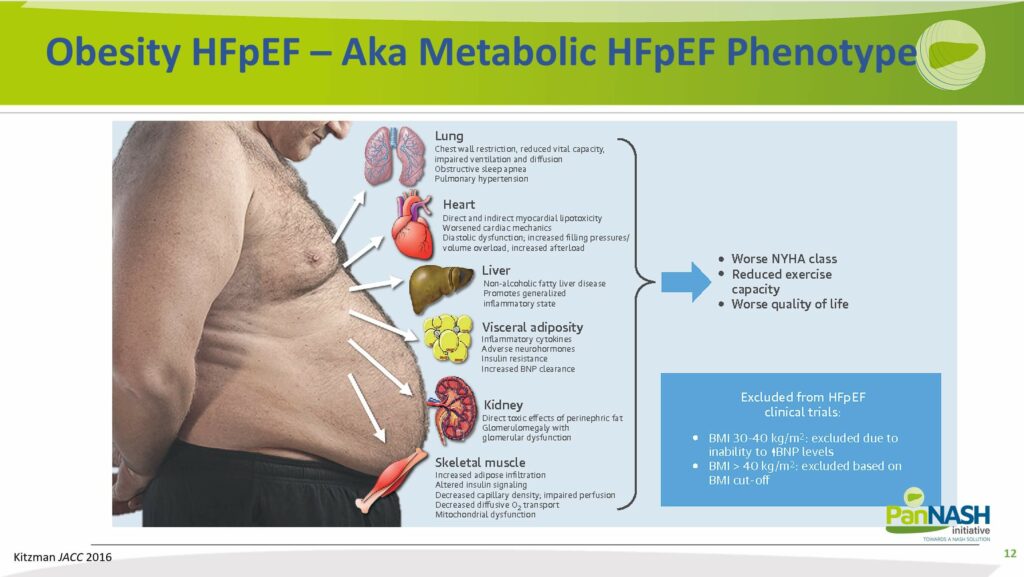
Obesity HFpEF – Also Known as Metabolic HFpEF Phenotypes
It’s important to acknowledge the undeniable influence of concurrent obesity and metabolic syndrome, factors driving both NAFLD and heart failure.
Later, when discussing management strategies for NAFLD and heart failure concurrently, it’s noteworthy that many of the successful or potentially successful treatments are not directly targeting the heart or even the liver. Instead, they primarily address metabolic syndrome, including hyperlipidemia and systemic inflammation. These are the factors that fuel the onset and progression of both conditions.
Therefore, a comprehensive focus on comorbid diseases is critical when dealing with both NAFLD and heart failure.
Screening for NAFLD
An interesting perspective on screening emerges when considering the regular interactions with heart failure patients as a cardiologist. Even though liver screening is not typically a top priority, well-established guidelines suggest otherwise.
These guidelines recommend that at-risk patients should be routinely scanned with a liver ultrasound even in a primary care setting. Risk factors include being over the age of 50, having diabetes, or exhibiting other features of metabolic syndrome. Concurrently, patients should also undergo liver enzyme evaluations to identify high-risk patterns.
Many cardiology practices, including the one of Dr Fudim, typically halt the process upon identifying elevated liver enzymes, fatty liver on ultrasound, or even cirrhotic liver. At this point, they generally refer the patient for further care.
However, given that about 25% of the US population alone is affected by NAFLD referring every patient with fatty liver to hepatologists would be overwhelming, as they do not have the capacity to handle such a large number of patients.
Therefore, the guidelines further recommend risk stratifying patients and obtaining a non-invasive risk score of fibrosis, such as the NFS or the FIB-4 score. These tools utilize biometric and laboratory data to risk stratify patients into low, intermediate, or high-risk categories for high-grade fibrosis.
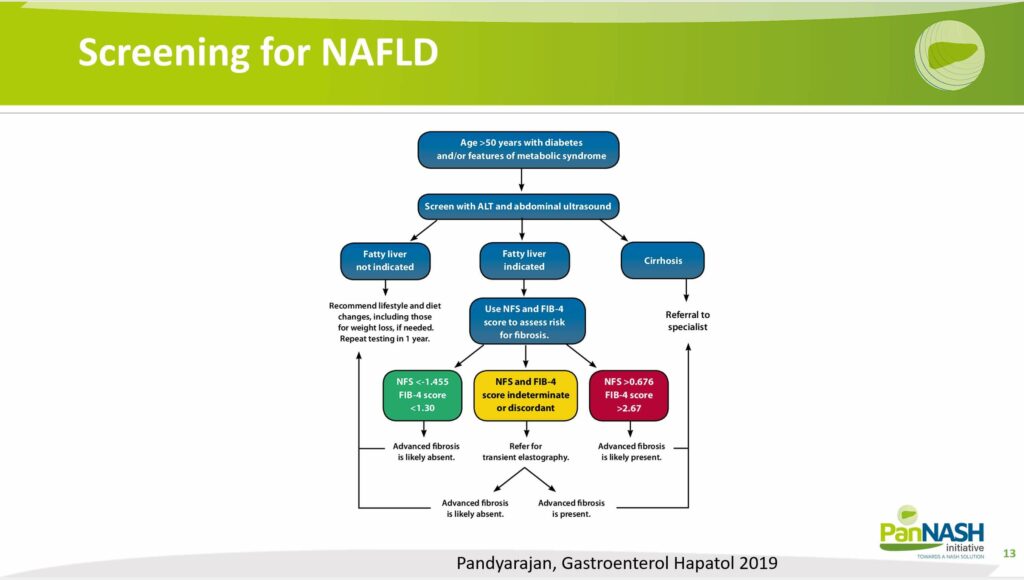
Subsequently, only those patients with high-risk fibrosis should be referred to liver disease centers for further management.
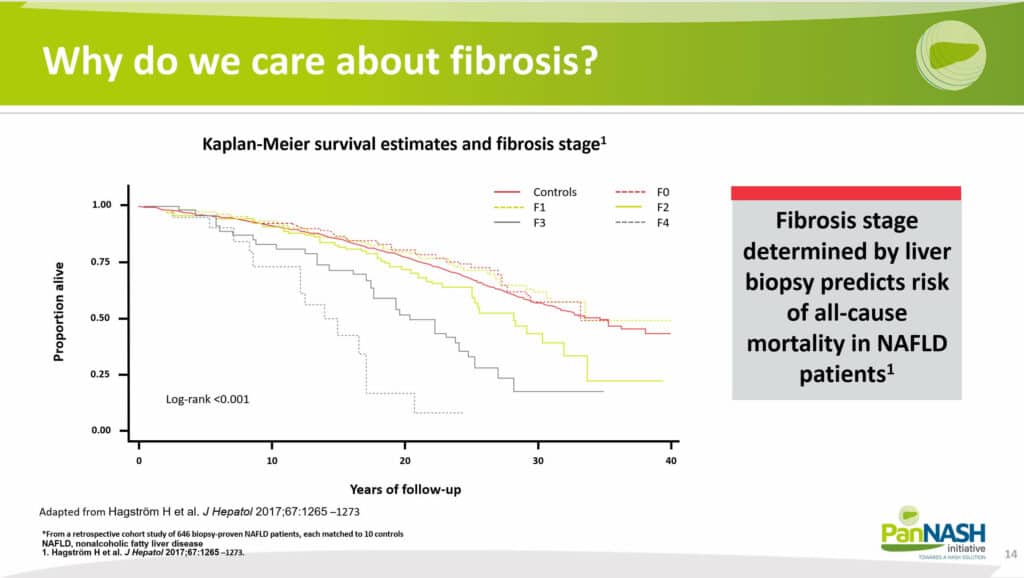
Why do we care about high-risk fibrosis?
The answer lies in the clear linear relationship between the degree of fibrosis and clinical outcomes. Fibrosis is graded from F0 (none) to F4 (the highest grade), and this grading directly correlates with patient survival rates.
Notably, patients with a high degree of fibrosis (F4) have the worst outcomes, as evidenced by their survival rates. Hence, upfront risk stratification can be extremely beneficial.
However, it’s doubtful whether this approach is adequately implemented in clinical practice, particularly concerning risk prediction for liver disease. In fact, the use of screening within cardiology practices appears to be highly underutilized.
There’s a significant need for further education on why it’s crucial to identify and screen for liver disease. Understanding the potential risks and implementing appropriate screening procedures can dramatically influence patient outcomes, particularly for those at high risk.
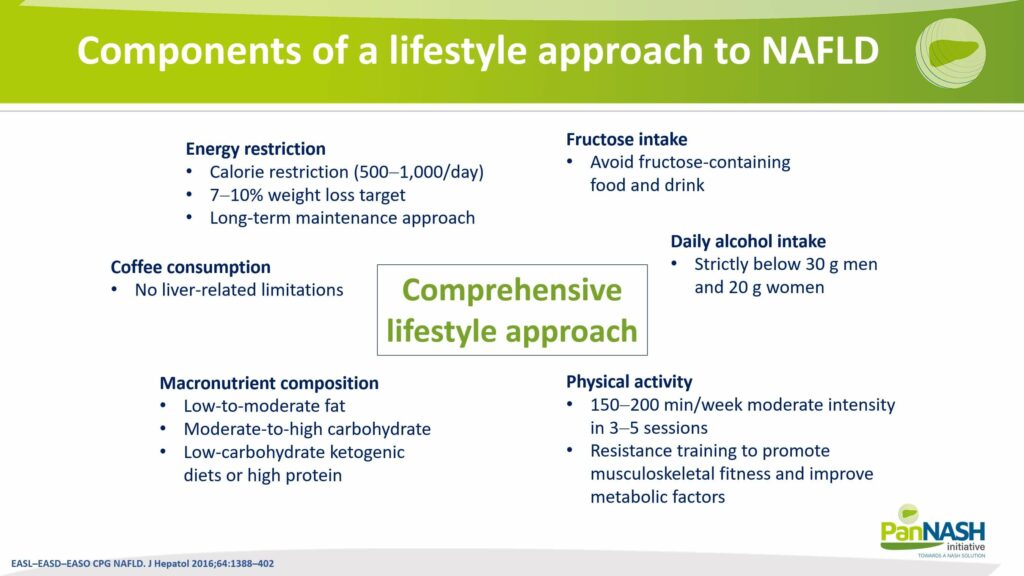
Components of a Lifestyle Approach to NAFLD
Upon identifying a patient with liver disease, what steps should be taken? The recommendations are quite similar to those for patients with heart failure, especially heart failure with preserved ejection fraction (HFpEF), where the focus is often on managing concomitant diseases, such as comorbidity.
Key recommendations include:
- Reducing alcohol intake: This helps protect the liver from further damage.
- Managing weight: Where applicable, losing weight can significantly reduce the stress on both the heart and liver. This can be achieved through various dietary approaches, such as a low-fat diet, a low-carbohydrate diet, or even a high-ketogenic diet.
There are numerous ways to implement lifestyle interventions to manage both non-alcoholic fatty liver disease (NAFLD) and HFpEF or HFrEF (heart failure with reduced ejection fraction).
However, it’s crucial to recognize these steps as the foundational cornerstones of both heart failure and NAFLD treatment. Hence, these lifestyle changes should always be implemented in parallel with any medical interventions.
Pharmacotherapy for NAFLD: Current Scenario and Approaches
Turning to pharmacological therapy, it’s important to acknowledge the current limitations. As of now, there are no approved therapies specifically for managing non-alcoholic steatohepatitis (NASH) that carry a high degree of evidence.
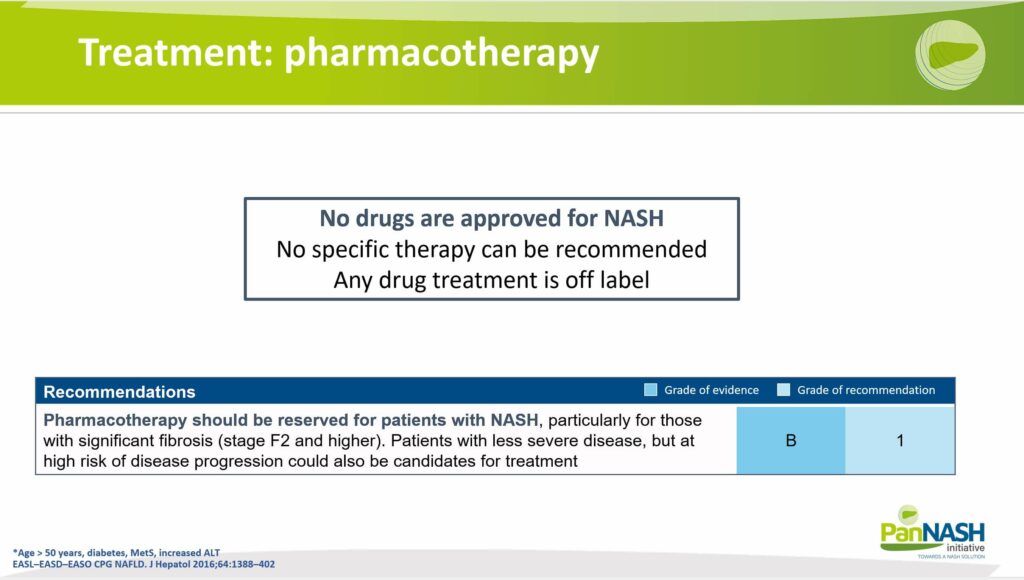
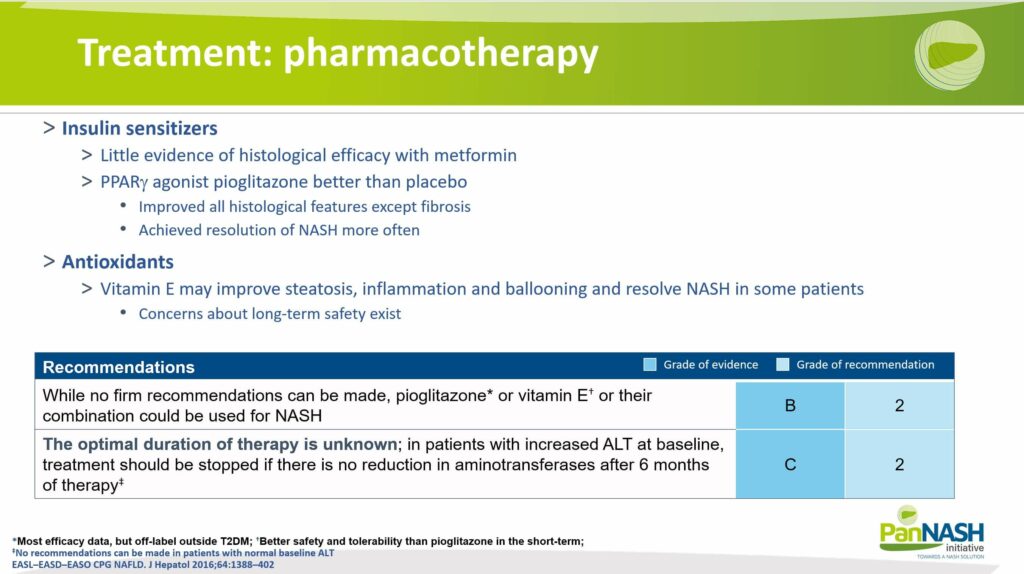
Many pharmacological therapies currently focus on managing the comorbid diseases associated with NAFLD. Several options show promise, albeit with a moderate level of evidence:
- PPAR-gamma drugs: These medications, typically used in the treatment of diabetes, have shown potential effects on NAFLD.
- Antioxidants: Certain antioxidants, like vitamin E, have been suggested to have beneficial effects on NAFLD, though the evidence supporting their use is currently moderate.
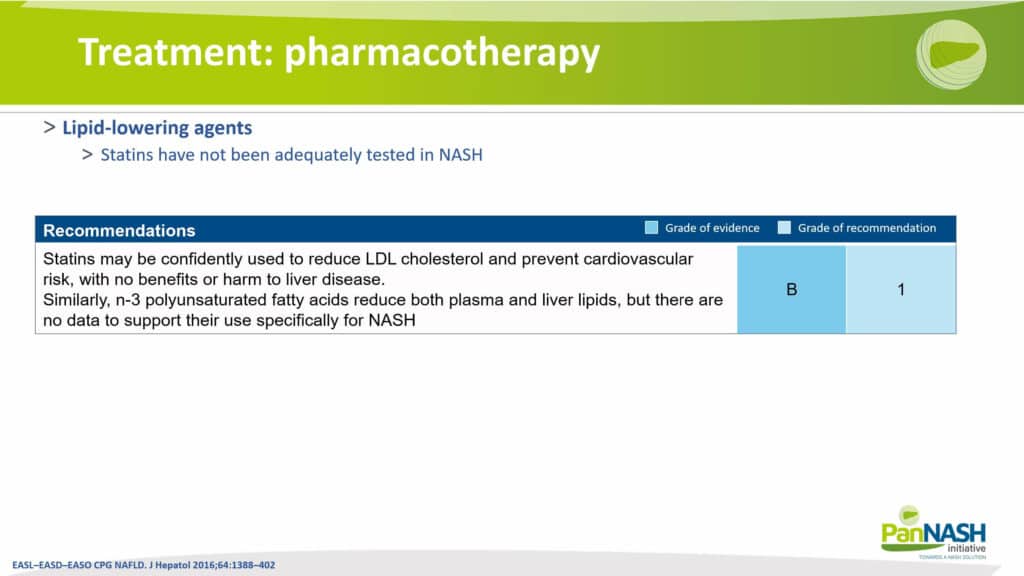
- Statins: These drugs are not directly targeted at the liver. However, their pleiotropic effects, including inflammation reduction, lipid level regulation, and reduction of coronary artery disease burden, might indirectly benefit NAFLD. Studies suggest some potential benefits of statins on NAFLD, further reinforcing their role in the management of this condition.
Given the evolving landscape of NAFLD treatment, it’s crucial to keep abreast of new research and treatment options. While the focus remains on managing comorbid conditions and lifestyle modifications, pharmacotherapy remains an essential part of the treatment approach.
Future Directions in NAFLD Pharmacotherapy: Mechanism of Action
To wrap up, it’s worth noting that while we currently have some treatments available for NAFLD, significant efforts are underway to develop novel therapies. These new treatments aim to target various pathophysiological mechanisms involved in NAFLD, such as:
- Inflammation: Medications that can effectively reduce liver inflammation may hold promise for improving NAFLD outcomes.
- Fibrosis: Treatments that can halt or reverse liver fibrosis, the excessive accumulation of scar tissue, could significantly impact disease progression.
- Lipid-altering therapies: As NAFLD is closely linked with abnormal lipid metabolism, drugs that can normalize this could be crucial in managing the disease.
- Insulin-sensitizing agents: Given the close relationship between NAFLD and insulin resistance, treatments that can enhance the body’s responsiveness to insulin may be beneficial.
These therapies, either alone or in combination, are expected to be introduced in the US and European markets in the future.
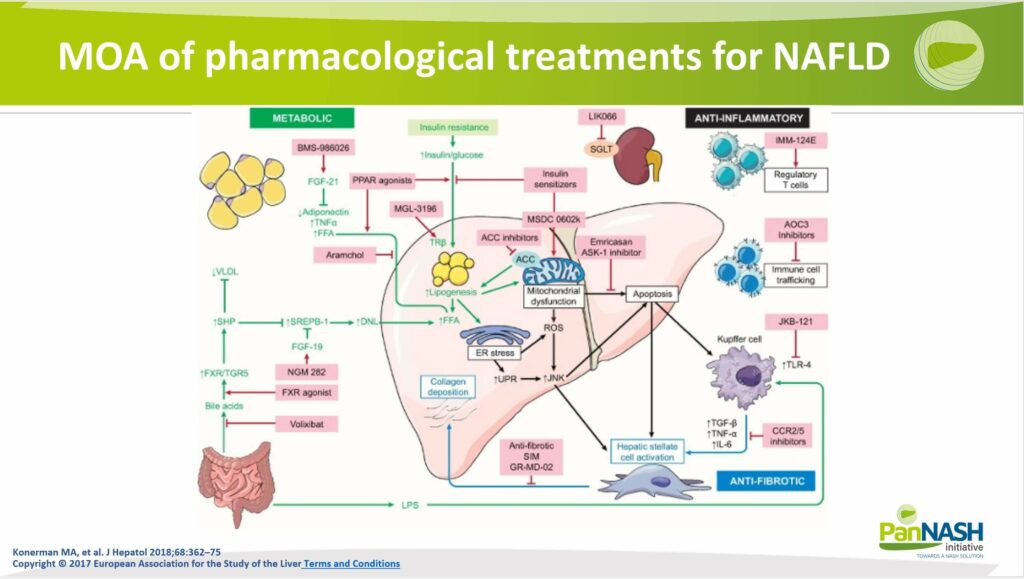
Looking ahead, the future appears quite promising for the field of NAFLD. The pharmaceutical industry has recognized the significant impact of NAFLD as a major risk factor for numerous diseases, particularly heart failure and cardiovascular diseases. Therefore, developing effective treatments for NAFLD has become a key focus.
Key Insights to Remember from Dr Marat Fudim
Let’s conclude with some crucial insights from Dr Marat Fudim’s discussion today:
- Overlap of Risk Profiles: Dr Fudim emphasizes that it’s become increasingly clear over the last few decades that non-alcoholic fatty liver disease (NAFLD) and heart failure share overlapping risk profiles.
- NAFLD as a Precedent: Emerging evidence suggests that NAFLD might not only be associated with heart failure but may indeed precede and contribute to its onset. Dr Fudim highlights the possibility of NAFLD being instrumental in the development of heart failure.
- Importance of Screening: Given these links, Dr Fudim stresses the importance for general practitioners, liver specialists, cardiologists, and heart failure specialists to screen for NAFLD.
- Therapeutic Landscape: Dr Fudim points out that while we currently lack many dedicated therapies for NAFLD, the pharmaceutical pipeline is rapidly filling up with novel pharmacological and non-pharmacological strategies targeting this disease.
- The Intersection of Treatment Approaches: Many of these emerging treatments for NAFLD also have potential applications in managing heart failure, as both conditions are fundamentally metabolic in nature. Dr Fudim considers this a promising development.
- Promoting Clinical Trials & Guidelines: Given these developments, Dr Fudim encourages the medical community to promote screening for NAFLD, consider enrolling patients in clinical trials, and stay updated on the latest clinical guidelines for treating and managing NAFLD.