Clinical Chemistry In NAFLD Part 3 – Biomarkers and Hepatic Fibrosis
INTRODUCTION ABOUT DR. GUILLAUME GRZYCH
Dr. Guillaume Grzych, an esteemed Associate Professor and Hospital Practitioner at the faculté de Pharmacie de Lille, illuminates the intricate dynamics of Clinical Chemistry in the field of Non-Alcoholic Fatty Liver Disease (NAFLD) in a crucial discussion.
Specializing in medical biology with a particular emphasis on biochemistry, Dr Grzych brings to the table an extensive reservoir of knowledge spanning not only the medical biological sciences but also pivoting into the realm of advanced computational techniques.
Dr. Grzych’s cross-disciplinary expertise places him at the forefront of modern medical research, and he is uniquely positioned to discuss the value and utility of biomarkers in NAFLD.
In this enlightening video series, Dr. Grzych endeavors to elucidate the precise concerns and focus of clinical chemists in the context of NAFLD. Articulated into three thoughtful segments, this series navigates through the pivotal concepts and discussions in the field. In this third and final installment, he will navigate through specific Biomarkers and Hepatic Fibrosis in NAFLD.
Table of Contents
- Exploring the Pathophysiology of Liver Fibrosis Through Biomarkers
- Utilizing the AST-to-ALT Ratio in Liver Disease Assessment
- Exploring FibroTest: A Costly yet Effective Liver Disease Diagnostic Tool
- APRI and FIB-4: Accessible Scoring Systems in Hepatic Fibrosis
- Analyzing the Efficacy of the NAFLD Fibrosis Score (NFS)
- the Viability of the BARD Score in Diagnosing Advanced Fibrosis
- Comprehensive Insight into the ELF Score and its Clinical Implications
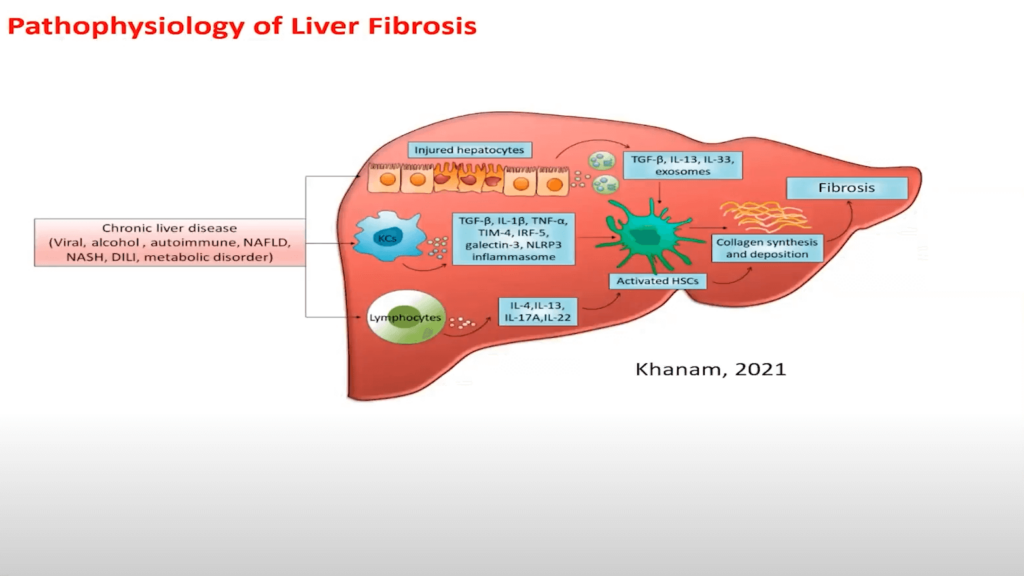
Exploring the Pathophysiology of Liver Fibrosis Through Biomarkers
Understanding hepatic fibrosis necessitates a deep dive into an array of available markers and combined marker scores, which are pivotal in determining the potential development of fibrosis in patients.
The pathophysiology’s nucleus demands our focus right at the outset, given that selecting an apt biomarker mandates profound knowledge in this domain. The etiology of liver fibrosis is multifaceted and can have myriad sources. These might envelop chronic liver disease stemming from various origins such as:
- Viral influences
- Alcohol
- Autoimmune factors
- NAFLD
Inflammation in the liver, albeit with elements of obfuscation in some instances, leads to the activation of certain cells. The cascade follows through the release of cytokines and proinflammatory signals, activating hepatic stellate cells (HSCs). The activated HSCs, as visually demonstrated on the following slide, expedite fibrosis through the synthesis of substances like collagen for exemple. Thus, we observe a plethora of potential biomarkers, which include:
- Proinflammatory biomarkers
- Biomarkers related to collagen synthesis
Diagnosing liver fibrosis might involve leveraging imaging or elastography techniques to measure liver stiffness. However, given their substantial cost and potential scarcity in certain hospitals or departments—due to the necessity of specific devices per patient—biomarkers present a compelling alternative. A plethora of biomarkers are available, comprising combinations of liver, inflammatory, and collagen fibrosis biomarkers.
A recent paper was reviewed by our specialized PanNash Authors Prof. Arun Sanyal, Prof. Laurent Castera and Prof. Vincent Wai-Sun Wong, provides a thorough exploration of non-invasive techniques related to liver fibrosis, with a specific focus on NAFLD. Today’s insights of Dr. Grzych on this topic are informed by their findings, and a comprehensive read of their work is recommended for a deeper, more nuanced understanding of this intricate subject matter.
Utilizing the AST-to-ALT Ratio in Liver Disease Assessment
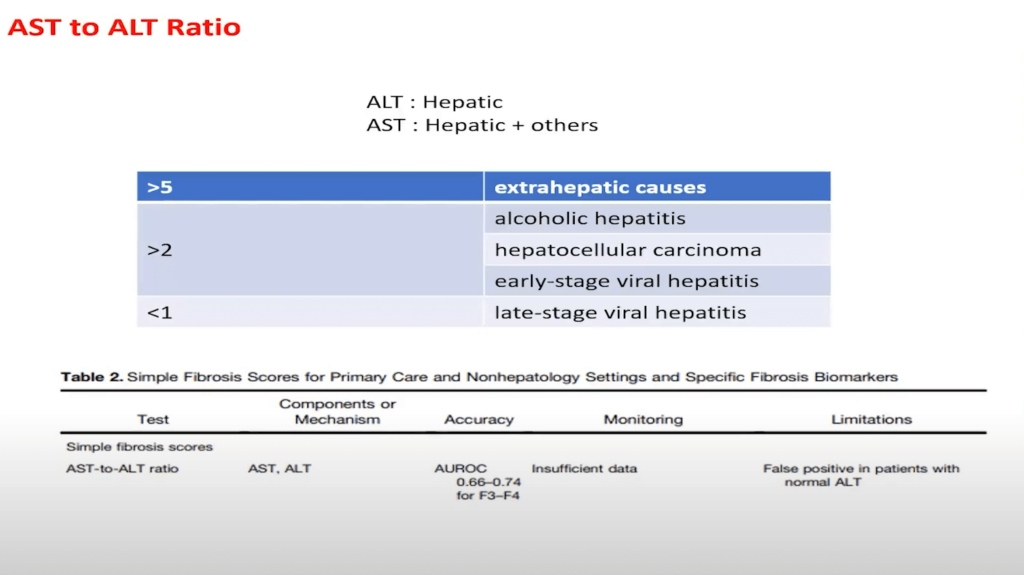
In the intricate landscape of liver disease diagnosis, Dr. Guillaume Grzych underscores the potential application of the AST-to-ALT ratio. Both transaminases, although utilized to navigate the complex realm of liver diseases, are not uniquely indicative of such conditions. ALT often emerges as more liver-specific compared to AST, which may elevate in situations such as hemolysis..It’s pivotal to recognize that these transaminases are not exclusive to liver disease. Whereas ALT is more liver-specific, AST can elevate in instances of hemolysis, thereby validating the importance of measuring and creating a ratio between the two transaminases. Notably, a higher elevation of ALT in comparison to AST is more indicative of liver specificity than other potential causes for transaminase elevation.
Utilizing this ratio when measuring transaminases in patients can assist healthcare professionals in distinguishing between liver and non-liver causes. For example, a significantly high score on this ratio, where AST surpasses ALT, might suggest an extrahepatic cause and ALT, in this scenario, becomes secondary—prompting a further investigation into alternative causes. A score hovering around two might be indicative of hepatitis, potentially NAFLD, or fibrosis.
However, according to a paper by our colleagues, the AST-to-ALT ratio provides insufficient data for diagnosing fibrosis, as it achieves an area under the curve of around 0.6, even with proficient external validation. The possibility of false positives in patients with normal ALT also exists, indicating that the utilization of transaminases might not be highly reliable. Particularly in more severe stages of NAFL, where fibrosis reduces hepatic cells and subsequently, enzyme cells, reliance on transaminase decreases, diminishing its effectiveness as a diagnostic tool.
Exploring FibroTest: A Costly yet Effective Liver Disease Diagnostic Tool
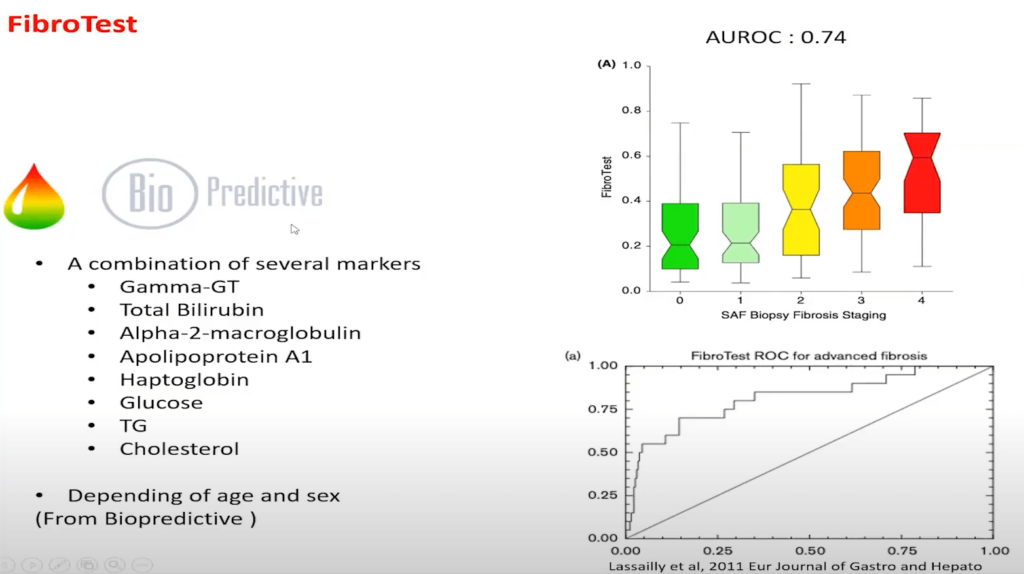
Navigating through the diagnostic tools available for liver diseases, Dr. Guillaume Grzych elucidates the utilization of FibroTest, a tool developed by the society Biopredictive. Incorporating markers that Dr. Grzych meticulously outlined in the second part of this video series, FibroTest operates on a secretive algorithm, demanding payment to unveil the results. Despite its concealment, its efficacy in diagnosing fibrosis—specifically, gauging its severity—is represented by a performance metric approximately between 0.7 and 0.74 when juxtaposed with histological tests. Dr. Grzych notes that a higher FibroTest result frequently correlates with a heightened severity observed in patient histology.
A gentle reminder from Dr. Grzych is to bear in mind the tangible costs and the necessity to measure an array of parameters with the FibroTest, positioning it as a potentially effective yet economically considerate option in liver disease diagnostics. This becomes a crucial aspect to ponder upon for healthcare practitioners, especially when balancing diagnostic accuracy with economic practicality in clinical settings.
APRI and FIB-4: Accessible Scoring Systems in Hepatic Fibrosis
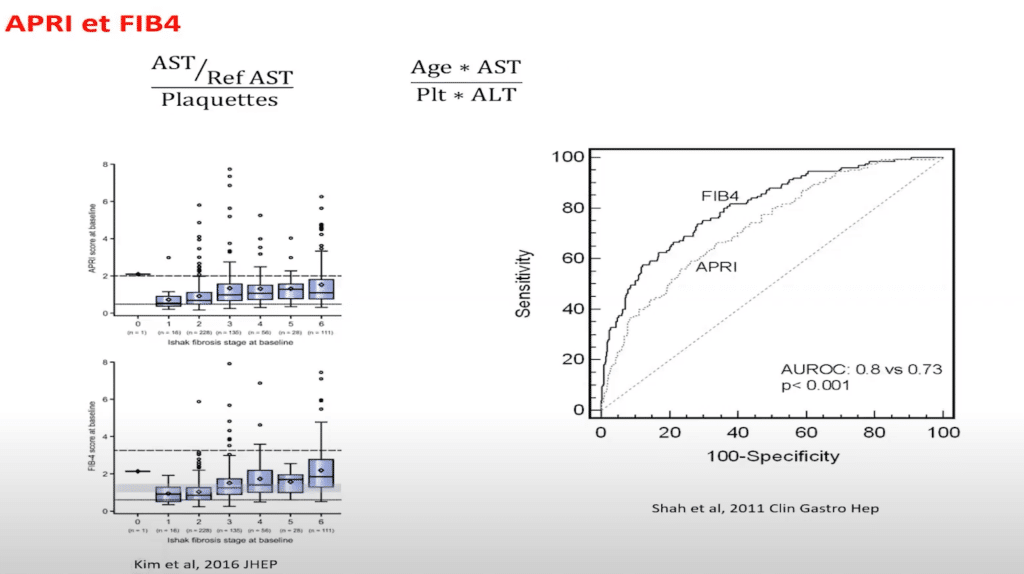
Dr. Guillaume Grzych dives into the exploration of APRI and FIB-4, revealing their notable relevance and application in diagnosing hepatic fibrosis. These scores, which utilize transaminases and platelets in their calculations, present themselves as potentially pivotal in the realm of liver disease diagnostics. But why platelets? Dr. Grzych explains that the liver plays a pivotal role in platelet synthesis by increasing Thrombopoietin (TPO), thus influencing platelet production. Consequently, liver issues can potentially manifest as a decrease in platelet numbers.
In evaluating performance, FIB-4, with external validation, demonstrates a compelling Area Under the Curve (AUC) of around 0.8, establishing it as a superior option compared to FibroTest, which garners an AUC close to 0.7 with similar external validation. The process to measure FIB-4 is markedly straightforward and perhaps safer, necessitating merely the age, transaminase, and platelets, in contrast to earlier requirements like Apolipoprotein and Haptoglobin. Often, only two biological parameters are needed, as transaminase is frequently measured concurrently, simplifying the approach to just two measurements and the patient’s age while ensuring robust performance. Consequently, it is recommended by esteemed entities, such as the EASL Society in Europe, to utilize FIB-4 to screen hepatic fibrosis in specific patients.
A recent paper by Dr. Grzych’s colleague, Laurent Castera, highlights the utility of FIB-4 in patients suspected to have NAFLD. Dr. Grzych emphasizes that this score isn’t designed for global screening in the general population; rather, it is suited for a specific patient demographic. Preliminary screening through clinical assessments and etiology identification is paramount, and in primary healthcare’s first line, FIB-4 can be utilized, with specific cutoffs dependent on age, to identify low-risk patients.
It’s essential to underscore that FIB-4 isn’t merely a diagnostic tool but also a management guide. For patients showcasing non-elevated FIB-4 numbers, lifestyle modifications and exercise can be implemented, with a reevaluation through FIB-4 after one year. If higher numbers are observed, indicating risk, referral to a hepatologist becomes imperative. This strategy, endorsed by liver societies and highlighted by Dr. Grzych, allows healthcare practitioners to strategically orient patients toward specialized hepatology consultation, potentially guiding them through further evaluations, such as transient elastography, to meticulously assess liver fibrosis. Its combined utility in diagnosis and patient care is endorsed by prominent liver societies, making it a valuable resource in liver disease management.
Analyzing the Efficacy of the NAFLD Fibrosis Score (NFS)
You have a better performance of NAFLD compared to APRI. But same, the same as FIB-4. But it’s good too. It’s a free score. So maybe you can combine the two score to have the same determination if you want to be sure if your patient has to be to go to the hepatologist. So it is a good score, also okay with liver society, recommended for liver society.
Dr. Guillaume Grzych brings to light another pivotal diagnostic tool – the NAFLD Fibrosis Score (NFS), which comes highly recommended by various liver health societies. There are various parameters in NFS, include:
- Age
- BMI (Body Mass Index)
- Glycemia/Diabetes levels
- Transaminase levels
- Platelet count
- Albumin levels
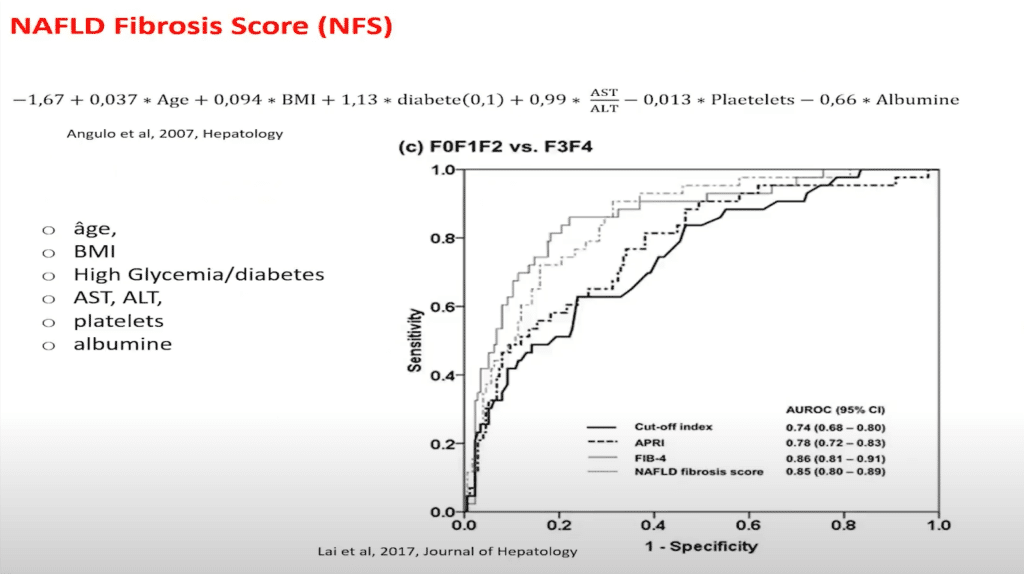
Dr. Grzych underscores the significant external validation data which contrasts low and high fibrosis patients, revealing NFS’s superior performance over APRI, mirroring FIB-4 metrics. Being effective and cost-efficient (a free score), NFS becomes an essential tool in liver disease diagnosis. Additionally, merging NFS and FIB-4 is suggested for augmented diagnostic accuracy, ensuring precise patient referrals and is endorsed by esteemed liver societies for its reliability in liver health diagnostics.
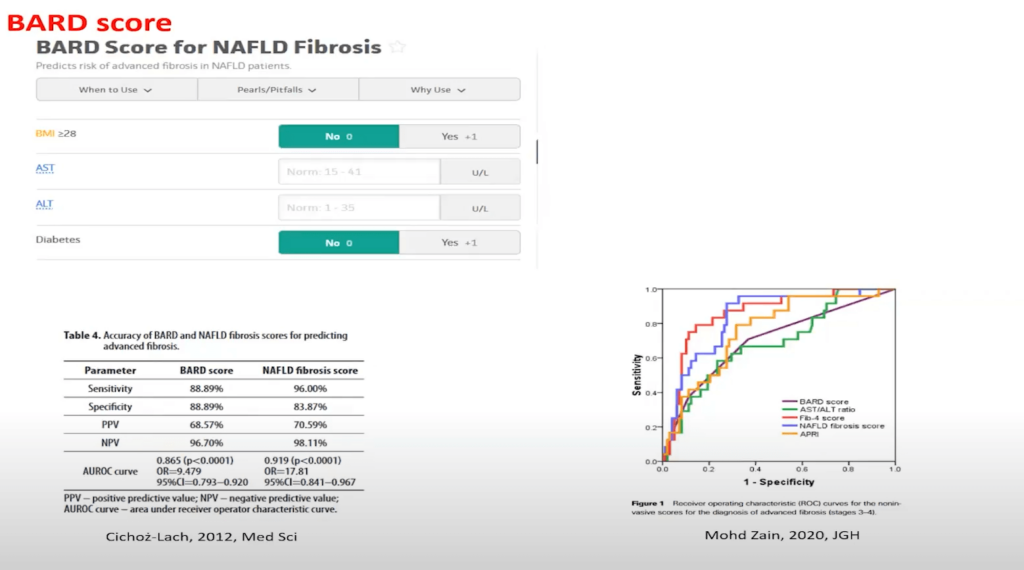
the Viability of the BARD Score in Diagnosing Advanced Fibrosis
In exploring alternative diagnostic tools, Dr. Guillaume Grzych introduces the BARD Score, a tool documented in medical literature for predicting the risk of advanced fibrosis in patients with NAFLD. The score uniquely synthesizes three key parameters in its algorithm:
- BMI
- Transaminase levels
- Diabetes
The displayed results indicate subpar performance by other scores compared to FIB-4 and NAFLD Fibrosis Score, even with high-performance liver conditions as seen in the discussed paper. Notably, the historical BARD score exhibits lesser efficacy. While both FIB-4 and NAFLD Fibrosis Score are recommended for primary health screening, it is crucial to note that their application is not universal for all patients. Particularly, when dealing with a large patient pool without specific indications, the performance of these scores hasn’t been evaluated, leaving a gap in understanding their efficacy for global screening populations.
Comprehensive Insight into the ELF Score and its Clinical Implications
Dr. Guillaume Grzych elucidates a crucial scoring system, known as the ELF Score (Enhanced Liver Fibrosis Score).
The ELF Score employs a confluence of biomarkers associated with fibrosis and collagen processes. Notably:
- Hyaluronic acids
- Inhibitor of metalloprotease 1
- Amino-terminal propeptide of type III procollagen. This particular component is directly linked to the synthesis processes of collagen and fibrosis.
A heightened ELF Score indicates a patient’s augmented risk of severe fibrosis. In terms of performance, the ELF Score showcases promising results with an area under the curve hovering around 0.83, as per meta-analysis data, thus underlining its efficacy in fibrosis identification.
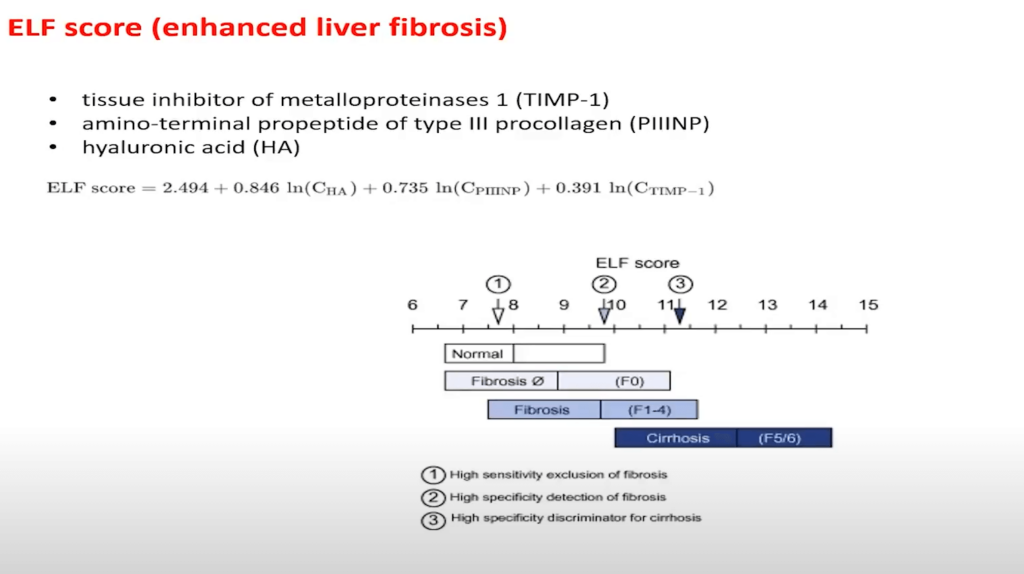
However, like every diagnostic tool, the ELF Score presents challenges:
Limitations:
- Marker Availability: A primary concern is the accessibility of specific markers. Some of these biomarkers are not routinely included in large automated analytical devices. This necessitates specialized labs in hospitals, making it challenging for widespread screening and availability.
- Relevance to General Population: The efficacy of the ELF Score depends significantly on the prevalence of NAFLD fibrosis in specific populations. There is a distinct difference in its application between primary care settings and specialized hepatology clinics. The performance of such non-invasive markers varies based on prevalence.
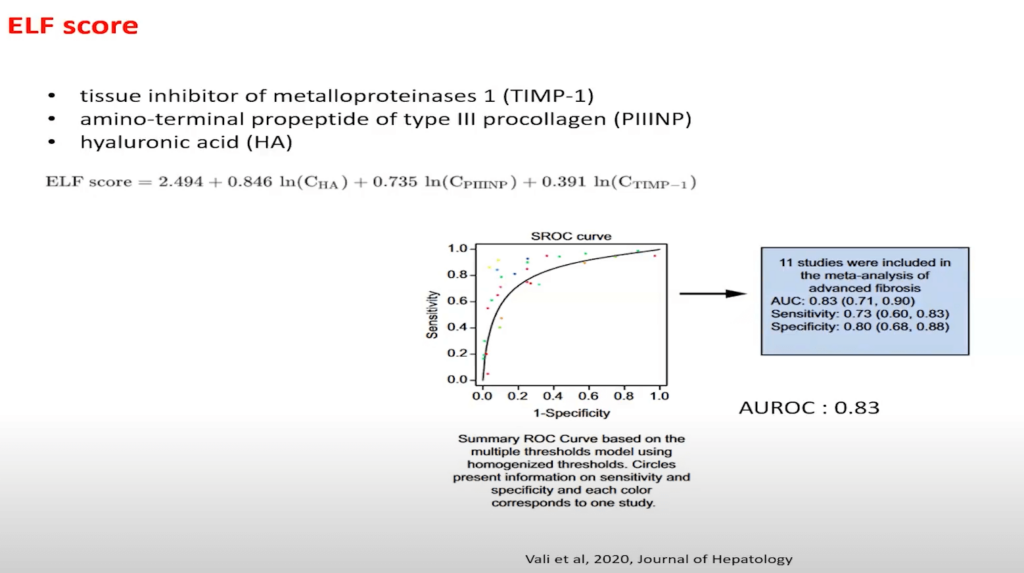
While the ELF Score has showcased its potential in specialized settings, its suitability for general screening remains a topic of debate. Dr. Grzych emphasizes the importance of interdisciplinary discussions involving clinicians, diabetes specialists, and hepatologists to determine the best diagnostic path for patients.
Summarizing NAFLD Biomarkers: Complexity and Interdisciplinary Approach
Dr. Guillaume Grzych highlights the significance of a variety of biomarkers available for diagnosing different stages of NAFLD with the following points:
- Biomarker Diversity: NAFLD diagnosis involves diverse biomarkers related to steatosis, NASH, and fibrosis.
- Disease Complexity: Given the complex nature of NAFLD, employing a combination of markers is essential for accurate diagnosis.
- Diagnostic Challenges: Single biomarkers or scores might not universally diagnose NAFLD effectively across different patients and disease stages.
- Importance of Collaboration: Effective diagnosis demands interdisciplinary cooperation among various specialists in the field.